Background: Indolent B-cell lymphomas are a group of neoplastic disorders that account for approximately one-third of non-Hodgkin lymphomas in the Western world. They are clinically indolent but pathologically diverse and generally composed of follicular lymphoma (FL), extranodal marginal zone lymphoma (EMZL), lymphoplasmacytic lymphoma (LPL), nodal marginal zone lymphoma (NMZL), splenic marginal zone lymphoma (SMZL), and small lymphocytic lymphoma. The overall prognosis is favorable in most patients, but others can have a more aggressive disease with associated progression, relapse, or histologic transformation. We have previously reported that the most common cause of death in FL was lymphoma. Here we report on the cause of death (COD), in other non-follicular indolent B-cell lymphomas (NFIBL) during the first decade of the rituximab era.
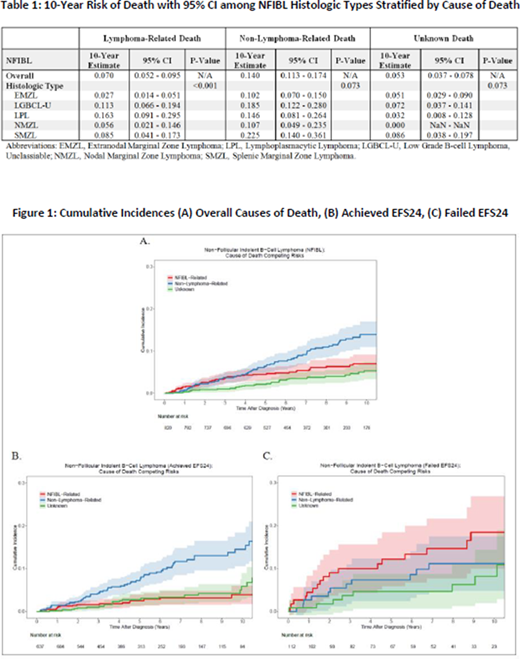
Methods: Participants were from the Molecular Epidemiology Resource (MER) of the University of Iowa/Mayo Clinic Lymphoma Specialized Program of Research Excellence (SPORE). From 2002 -2015, MER offered enrollment to all patients with newly diagnosed lymphoma who were US residents and age >18 years. Patients were treated per physician choice and followed prospectively. An event was defined as progression or relapse, initiation of 2nd line therapy, or death from any cause. EFS24 was defined using event-free survival at 24 months from diagnosis. Overall survival was defined as the time from diagnosis until death due to any cause. Overall survival from EFS24 was defined as time from event defining date (achieving EFS24 or early event). For decendents, copies of the death certificate or medical records associated with death were reviewed. Cumulative incidence estimates of the cause of death in NFIBL were calculated as competing risks utilizing the cuminc function from the cmprsk package in R version 3.6.2. COD was categorized as a result of lymphoma (progression or therapy-related) vs. other causes vs. unknown/missing. Results: 820 patients with newly diagnosed NFIBL were enrolled in this study. The subtypes included extranodal marginal zone (EMZL, N = 362), unclassifiable low-grade B-cell lymphoma (LGBCL-U, N = 202), lymphoplasmacytic lymphoma (LPL, N = 92), nodal marginal zone lymphoma (NMZL, N = 80), and splenic marginal zone lymphoma (SMZL, N = 84). The median age at diagnosis was 63 years (range 18-92), and 50.5% were male. Baseline clinicopathologic characteristics showed that the LDH was abnormal in 19.3%, hemoglobin was abnormal in 33.8%, and 62.8% had stage III-IV disease. The IPI score was 0-1 in 51%, 2 in 36.6%, 3 in 10.6%, and 4-5 in 1.8%. At a median follow-up of 83 months (range 0-193), 172 (21%) patients had died, and the primary cause of death was non-lymphoma related in 87 (50.6%), lymphoma related 48 (27.9%), and unknown in 37 (21.5%). When examining all subtypes combined, the 10-year estimate for lymphoma related death was 7% (95% CI: 5.2-9.5) which was lower than the rate of non-lymphoma related death (10 years estimate 14%, 95% CI: 11.3-17.4), Figure 1A, Table 1. The 10-year estimate of lymphoma related death varied by subtype, ranging from 2.7% in EMZL to 16.3% in LPL (table 1), while non-lymphoma related death at 10 years ranged from 10.2% in EMZL to 22.5% in SMZL; only in LPL was the lymphoma related rate higher than the non-lymphoma. Patients who failed to achieve EFS24 from diagnosis had significantly higher rates of lymphoma related death (18% at 10 years from failure, 95% CI: 11.7-29.1, Figure 1B) compared to patients who achieved EFS24 (3.9% at 10 years from achieving EFS24, 95% CI: 2.3-6.8, Figure 1C). Rates were similar by EFS24 for non-lymphoma related death (14.5%, 95% CI: 11.0-19.0 vs. 11.2, 95% CI: 6.3-19.7). Figure 1B-C.
Conclusion: The most common cause of death in NFIBL at 10 years was unrelated to lymphoma, in contrast to our previous data in follicular lymphoma which showed lymphoma as the most common cause of death at 10 years. However, similar to follicular lymphoma, patients with NFIBL who failed to achieve EFS24 to frontline therapy had significantly increased risk of lymphoma related death. Further research into the cause of death in NFIBL is warranted.
Maurer:Celgene / BMS: Research Funding; Morphosys: Membership on an entity's Board of Directors or advisory committees; Kite: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Nanostring: Research Funding. Witzig:Celgene: Consultancy, Research Funding; MorphSys: Consultancy; AbbVie: Consultancy; Incyte: Consultancy; Acerta: Research Funding; Karyopharm Therapeutics: Research Funding; Immune Design: Research Funding; Spectrum: Consultancy. Novak:Celgene/BMS: Research Funding. Farooq:Kite, a Gilead Company: Honoraria. Cerhan:BMS/Celgene: Research Funding; NanoString: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.